Research in the past few decades has revealed a link between alpha-synuclein aggregates in the brain and neurodegenerative diseases such as Parkinson’s. Until recently, though, scientists have not understood how those aggregates originate and spread. But a new experimental study using transgenic mouse models may change that. Researchers are hopeful that this new understanding of how alpha-synuclein aggregates spread could lead to future treatment breakthroughs for Parkinson’s disease and other debilitating neurodegenerative conditions.
Alpha-Synuclein Aggregates and Parkinson’s
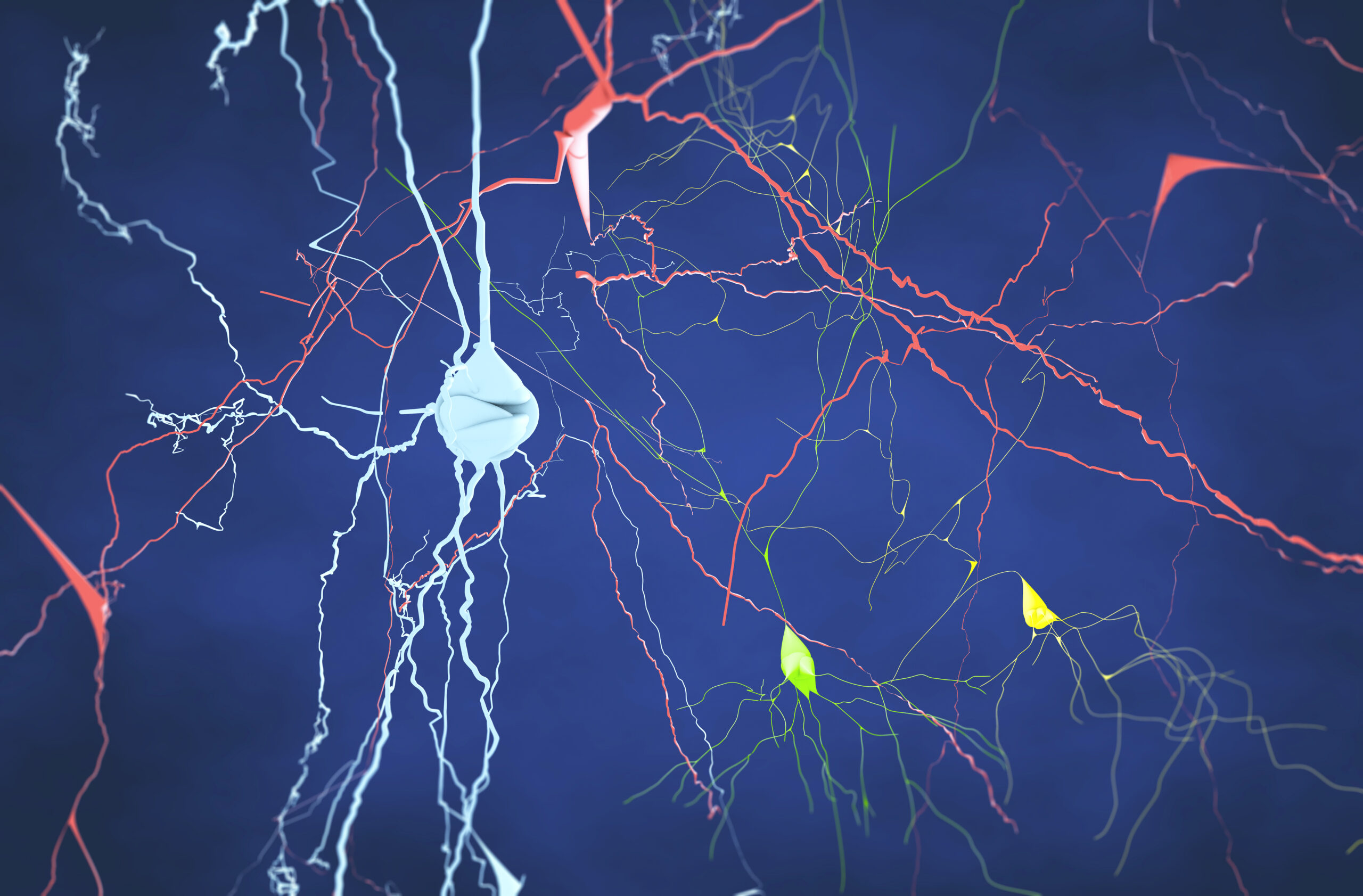
In the last few decades of research, scientists have observed the brains of transgenic mouse models and other animal models to understand how Parkinson’s disease grows and spreads in the brain. One of the primary findings of this research has been the observable link between Parkinson’s disease and the abnormal growth and spread of neuronal proteins known as alpha-synuclein aggregates.
Using transgenic mouse models and animal models, researchers have observed that in Parkinson’s disease, alpha-synuclein aggregates grow and spread exponentially throughout the brain, moving and expanding in an infection-like chain reaction. As these alpha-synuclein aggregates grow larger, they are able to induce more and more normal alpha-synuclein proteins to join them in an ever-growing aggregate. Large aggregates eventually break off into smaller aggregates, which continue the same process of growing and spreading throughout the brain.
Researchers have demonstrated that it’s possible to induce exponential alpha-synuclein aggregate spread by injecting alpha-synuclein aggregates into the transgenic mouse models’ brains as well as other animal models’ brains. Until recently, however, scientists have not understood the mechanisms by which alpha-synuclein aggregates spread from one neuron to another — only that they do.
Now, we may be one step closer to understanding how alpha-synuclein originates and spreads through neurons thanks to a new study published in Nature Communications. The research team was led by Dr. Manu Sharma, assistant professor of neuroscience at the Feil Family Brain and Mind Research Institute and Appel Alzheimer’s Disease Research Institute at Weill Cornell Medicine, and co-first author Ying Xue Xie, a doctoral candidate in the Weill Cornell Graduate School of Medical Sciences.
Exploring the Breakthrough
Using an alpha-synuclein A53T transgenic mouse (hA53Ttg) model, Dr. Sharma and his team learned that alpha-synuclein aggregates originate within the neurons themselves, but that, critically, they accumulate and spread through lysosomes.
In a healthy brain, lysosomes contain enzymes that can digest and recycle proteins and molecular waste into their own building blocks. But Dr. Sharma and his team observed that lysosomes were not capable of efficiently breaking down alpha-synuclein aggregates due to their tightly knit amyloid structure.
In the study, Dr. Sharma’s team observed that, instead of breaking down the alpha-synuclein aggregates, the lysosomes were observed to often “dump” the aggregates from the neurons they originated from instead. This process, known as exocytosis, influenced the further accumulation of alpha-synuclein aggregates. As a lysosome in the transgenic mouse models’ brains would encounter alpha-synuclein aggregates, the lysosome would migrate to and merge with the cell membrane, causing lysosome contents to be released, unencapsulated, into the fluid around the cell itself.
The research team was further able to demonstrate that by slowing the rate of lysosomal exocytosis, they were also able to reduce the concentration of alpha-synuclein aggregates capable of spreading. This is where, as Dr. Sharma explains, there is hope for a potential future breakthrough in the treatment of Parkinson’s — and other neurodegenerative diseases, too. Lysosomal exocytosis may be a viable target for treatments and preventives for a variety of disorders. In fact, Dr. Sharma and his team are currently building on this research by studying the roles of lysosomes in Alzheimer’s disease.
Scantox is a part of Scantox, a GLP/GCP-compliant contract research organization (CRO) delivering the highest grade of Discovery, Regulatory Toxicology and CMC/Analytical services since 1977. Scantox focuses on preclinical studies related to central nervous system (CNS) diseases, rare diseases, and mental disorders. With highly predictive disease models available on site and unparalleled preclinical experience, Scantox can handle most CNS drug development needs for biopharmaceutical companies of all sizes. For more information about Scantox, visit www.scantox.com.